- For Appointment : +91-9330257079
- +91-9830636315
-
bodhi.doc@gmail.com
What is Osteoporosis:
The word 'osteoporosis' means 'porous bone.' It is a disease that weakens bones, and if you have it, you are at a greater risk for sudden and unexpected bone fractures. Osteoporosis means that you have less bone mass and strength. The disease often develops without any symptoms or pain, and it is usually not discovered until the weakened bones cause painful fractures. Most of these are fractures of the hip, wrist and spine.
What are the symptoms of Osteoporosis:
There typically are no symptoms in the early stages of bone loss. But once your bones have been weakened by osteoporosis, you might have signs and symptoms that include:
>>Back pain, caused by a fractured or collapsed vertebra
>>Loss of height over time
>>A stooped posture
>>A bone that breaks much more easily than expected
What causes Osteoporosis:
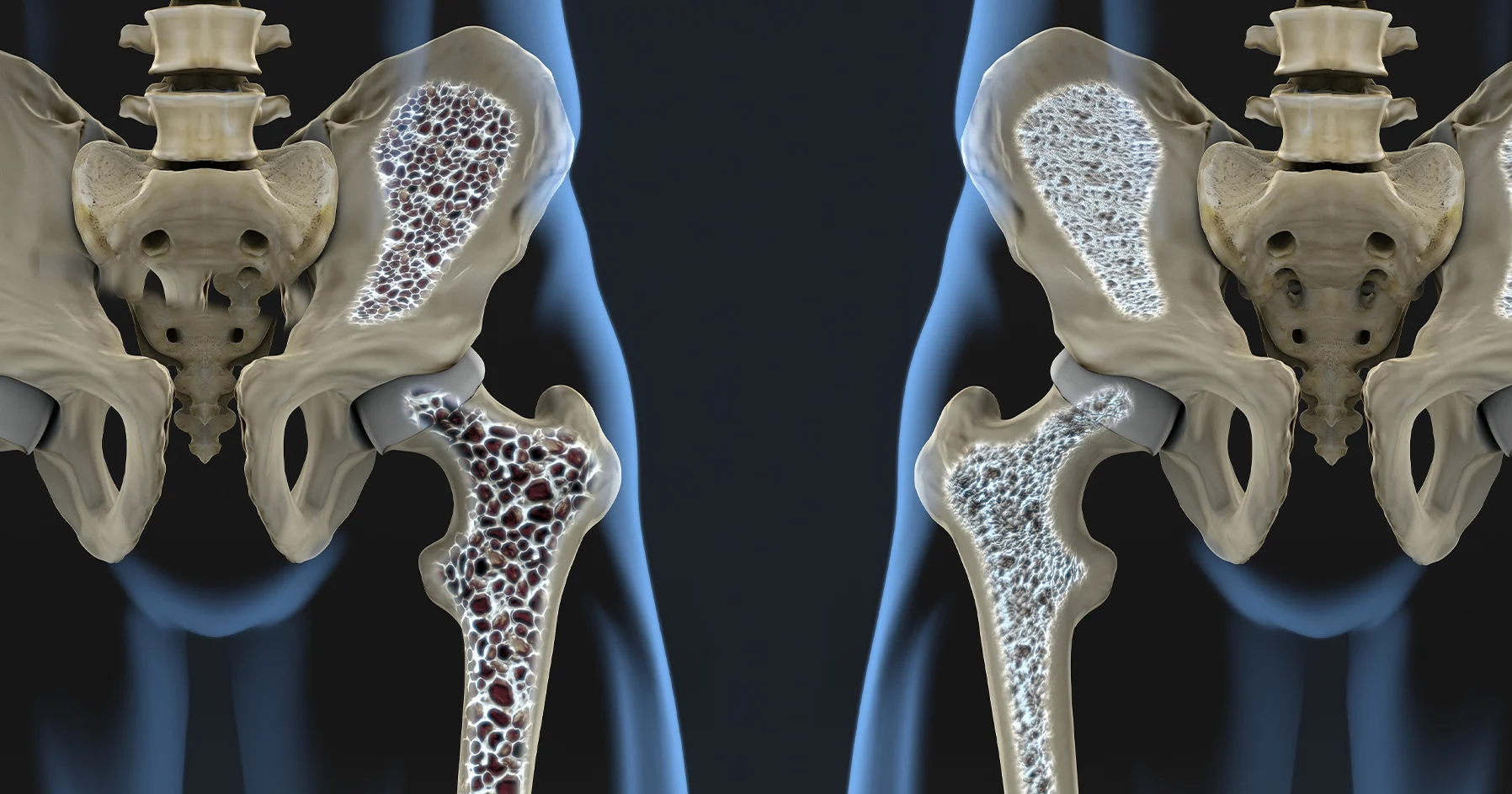
Researchers understand how osteoporosis develops even without knowing the exact cause of why it develops. Your bones are made of living, growing tissue. The inside of healthy bone looks like a sponge. This area is called trabecular bone. An outer shell of dense bone wraps around the spongy bone. This hard shell is called cortical bone.
When osteoporosis occurs, the "holes" in the "sponge" grow larger and more numerous, which weakens the inside of the bone. Bones support the body and protect vital organs. Bones also store calcium and other minerals. When the body needs calcium, it breaks down and rebuilds bone. This process, called bone remodeling, supplies the body with needed calcium while keeping the bones strong.
Up until about age 30, you normally build more bone than you lose. After age 35, bone breakdown occurs faster than bone buildup, which causes a gradual loss of bone mass. If you have osteoporosis, you lose bone mass at a greater rate. After menopause, the rate of bone breakdown occurs even more quickly.
Who is at risk for developing Osteoporosis:
There are many risk factors that increase your chance of developing osteoporosis, with two of the most significant being gender and age.
Everyone's risk for osteoporosis fractures increases with age. However, women over the age of 50 or postmenopausal women have the greatest risk of developing osteoporosis. Women undergo rapid bone loss in the first 10 years after entering menopause, because menopause slows the production of estrogen, a hormone that protects against excessive bone loss.
Age and osteoporosis affect men also. You might be surprised to know that men over the age of 50 are more likely to have an osteoporosis-induced bone break than to get prostate cancer. About 80,000 men per year are expected to break a hip, and men are more likely than women to die in the year after a hip fracture.
Another factor is bone structure and body weight. Petite and thin people have a greater risk of developing osteoporosis because they have less bone to lose than people with more body weight and larger frames.
Family history also plays a part in osteoporosis risk. If your parents or grandparents have had any signs of osteoporosis, such as a fractured hip after a minor fall, you may have a greater risk of developing the disease.
Finally, some medical conditions and medications increase your risk. If you have or had any of the following conditions, some of which are related to irregular hormone levels, you and your healthcare provider might consider earlier screening for osteoporosis.
>>Overactive thyroid, parathyroid, or adrenal glands.
>>History of bariatric (weight loss) surgery or organ transplant.
>>Hormone treatment for breast or prostate cancer or a history of missed periods.
>>Celiac disease, or inflammatory bowel disease.
>>Blood diseases such as multiple myeloma.
Some medications cause side effects that may damage bone and lead to osteoporosis. These include steroids, treatments for breast cancer, and medications for treating seizures. You should speak with your healthcare provider or pharmacist about the effect of your medications on bones.
It may seem as though every risk factor is related to something that is out of your control, but that's not true. You do have control over some of the risk factors for osteoporosis. You can discuss medication issues with your healthcare provider. And-you are in charge of your:
Eating habits: You are more likely to develop osteoporosis if your body doesn't have enough calcium and vitamin D. Although eating disorders like bulimia or anorexia are risk factors, they can be treated.
Lifestyle: People who lead sedentary (inactive) lifestyles have a higher risk of osteoporosis.
Tobacco use: Smoking increases the risk of fractures.
Alcohol use: Having two drinks a day (or more) increases the risk of osteoporosis.
How Osteoporosis is diagnosed:
Your healthcare provider can order a test to give you information about your bone health before problems begin. Bone mineral density (BMD) tests are also known as dual-energy X-ray absorptiometry (DEXA or DXA) scans. These X-rays use very small amounts of radiation to determine how solid the bones of the spine, hip or wrist are. Regular X-rays will only show osteoporosis when the disease is very far along.
All women over the age of 65 should have a bone density test. The DEXA scan may be done earlier for women who have risk factors for osteoporosis. Men over age 70, or younger men with risk factors, should also consider getting a bone density test.
A bone density test can help you determine if you have osteoporosis or are at risk.
How do you know if you have osteoporosis or if you are at risk? This is a common question, and one to get answered sooner rather than later.
Because bone loss typically happens gradually and painlessly, the first sign of osteoporosis can be breaking a bone, often more easily than you'd expect. But it is possible to determine if you have osteoporosis, even before a bone is broken, by getting a bone density test. The test can also detect if your bone density is lower than normal for a person of your age and sex. Bone loss that has not reached the stage of an osteoporosis diagnosis is called osteopenia.
Bone density testing
A bone density test is as close as your doctor can come to predicting your future bone health. The test results will show if you have osteopenia or osteoporosis, and how susceptible your bones are to fracture. A bone density test is the best way to predict fracture risk.
The test uses X-rays to measure how many grams of calcium and other bone minerals are in a square centimeter of bone. Generally, the higher the mineral content, the denser the bone is. And the denser bones are, the less likely they are to fracture.
Bone density testing uses a device called a bone densitometer. Most densitometers measure how much of a low-energy X-ray beam is absorbed as it passes through bone, in comparison to the absorption as the beam passes through the soft tissues next to the bone. The amount of X-ray energy that enters the bone is also compared with the amount of energy that leaves the bone. Denser bone absorbs more of the X-ray beam.
Central densitometers
These machines, typically found in hospitals and medical centers, are used to measure the density of the central, stabilizing parts of the skeleton, such as the spine and hip. This type of densitometer provides the most accurate bone density testing and can predict your potential risk of fracture.
Dual energy X-ray absorptiometry (DXA). A DXA machine uses two different X-ray beams to increase the precision of what it's measuring. As you lie on a padded platform, two mechanical arms containing an X-ray source and detector above and below your body are aligned. DXA is most often performed on the narrow neck of the upper leg bone (femur), just below the hip joint, as well as the lumbar vertebrae, which form the lower part of the spine. DXA testing is painless and takes only a few minutes.
Quantitative computerized tomography (QCT). This instrument measures bone density using computerized tomography (CT). Similar to having a CT scan, you lie on a movable padded table that slides into a large cylinder, where X-ray images are obtained from all angles. QCT is most often used to measure density in the vertebrae and the part of the femur below the hip.
Peripheral densitometers
Smaller devices are used to measure bone density on the periphery of the skeleton, such as in the wrist and heel bone. Although they are more portable, these densitometers are less accurate at predicting fracture risk. If your test on a peripheral device is positive for osteopenia or osteoporosis, then your doctor might recommend a follow-up scan of your spine or hip to confirm the diagnosis.
Quantitative ultrasound (QUS). This procedure is often called heel ultrasound because it typically measures bone density in the heel bone. Instead of X-ray radiation, QUS sends high-frequency sound waves through your heel while you rest your bare foot on the instrument. This type of densitometer measures the reflection of sound waves. Denser bone reflects sound waves back to the device sooner.
Peripheral dual energy X-ray absorptiometry (pDXA). This device is a compact, portable DXA scanner. Using X-rays, pDXA measures bone density in the wrist or heel. Although it's quick and accurate, this testing can be expensive.
Peripheral quantitative computerized tomography (pQCT). This portable version of QCT measures the bone density of the wrist or hand. This test is also expensive, and it produces a higher radiation exposure than do other tests.
Other types of testing, including 3-D imaging and high-resolution magnetic resonance imaging (MRI), are also under investigation.
When should you call the doctor about osteoporosis?
If you have risk factors and are concerned about osteoporosis, ask your healthcare provider about being screened, even if you are not as old as 65 (for women) or 70 (for men). Osteoporosis can be serious. Fractures can alter or threaten your life. A significant number of people have osteoporosis and have hip fractures die within one year of the fracture. Always call your healthcare provider if you fall, if you are worried about bone breaks, or if you have back pain that is severe that comes on suddenly.
Remember that you are able to lead an active and fulfilling life even if you do have osteoporosis. You and your healthcare provider can work together to make this happen.
