- For Appointment : +91-9330257079
- +91-9830636315
-
bodhi.doc@gmail.com
Specialist Rheumatological Consultation:
Rheumatology focuses on conditions where the immune system, inflammation, or joint degeneration causes pain, swelling, stiffness, or damage over time. Many patients spend months treating symptoms without a clear diagnosis. This consultation is designed to find the cause early and treat it properly.
Conditions commonly managed
• Inflammatory arthritis: Rheumatoid arthritis, Psoriatic arthritis, Ankylosing spondylitis / Spondyloarthritis
• Degenerative joint disease: Osteoarthritis (knee, hip, spine, shoulder)
• Autoimmune/connective tissue diseases: Lupus (SLE), Sjogren’s, Systemic sclerosis and related disorders
• Crystal arthritis: Gout, Pseudogout
• Soft-tissue pain conditions: Frozen shoulder, bursitis, tendinitis, tennis elbow, plantar fasciitis, fibromyalgia
• Chronic back/neck pain (including inflammatory patterns)
What you can expect
• A clear explanation of your diagnosis (often with simple visuals)
• A plan balancing evidence + safety + your lifestyle and budget
• Guidance on medicines, injections (if needed), exercise/physio, precautions, and follow-up


Specialist Medicine Consultation:
This is for general medical problems and long-term disease management where you want structured, sensible care with necessary tests and without “trial-and-error” medicines. It’s especially useful when multiple issues overlap, like thyroid + BP + diabetes + fatigue + recurrent infections, where one problem can worsen another, and treatment needs to be coordinated.
You’ll get a plan that is practical, easy to follow, and aligned to your daily routine.
Common conditions managed
• Hypertension, diabetes, thyroid disorders
• Fever/infection work-up (including dengue/chikungunya/viral illnesses)
• Asthma/COPD, allergies
• Cardiac risk management, headache/migraine, electrolyte disturbances
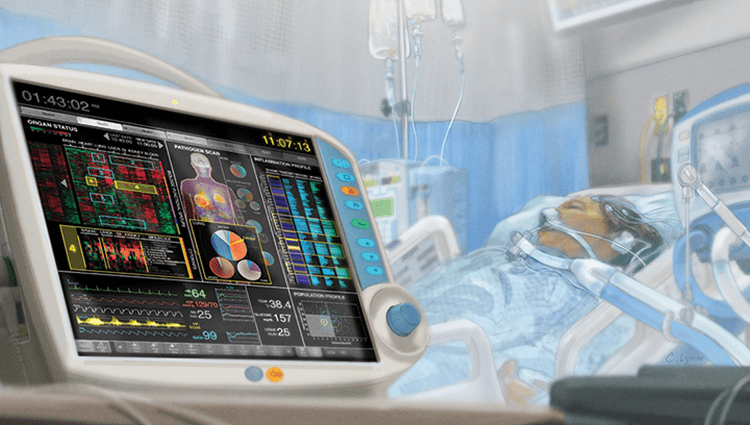
Specialist Critical Care Consultation
Critical care focuses on the management of seriously ill patients who need close monitoring, ICU-level decision-making, ventilator/hemodynamic support, and time-sensitive interventions. Many ICU outcomes improve when decisions are made early, systematically, and communicated clearly.
I also ensure family counselling is structured and consistent, because confusion and mixed messages often add unnecessary stress during ICU care.
Conditions commonly managed
• Sepsis, septic shock, ARDS
• Severe pneumonia, COPD exacerbations, respiratory failure
• Complicated dengue/malaria and multi-organ dysfunction
• Heart attack/heart failure, stroke, meningitis/encephalitis
• Acute kidney injury, dialysis support, severe electrolyte/acid-base disorders
• Critical poisoning / metabolic emergencies

Interventional Rheumatology (Procedures & Advanced Injections)
Modern rheumatology isn’t only about tablets. Many joint and soft-tissue problems improve faster (and more safely) when we treat the exact structure causing pain, joint lining, bursa, tendon sheath, enthesis, or a trapped nerve, rather than “blanket” painkillers.
Interventional rheumatology brings precision into patient care:
• Faster relief in painful flares (so you can move, sleep, and function again)
• Better accuracy with ultrasound-guided procedures (especially for deeper joints and tendon sheaths)
• Helps reduce repeated high-dose painkillers and their side effects
• Often prevents a “small untreated problem” from becoming a long-lasting disability
• Improves diagnosis and prevents wrong treatment
This approach is now a key part of modern rheumatology because it improves diagnostic confidence (what exactly is inflamed) and provides faster symptom control, often reducing the need for repeated oral painkillers.
What procedures may include
Diagnostic & therapeutic aspiration: removing excess joint fluid/bursal fluid (often gives immediate relief) and sending it for testing when needed
• Targeted injections (when indicated): intra-articular / peri-articular injections for inflammation and pain control
• Bursa / tendon-sheath / enthesis injections: e.g., frozen shoulder, tennis elbow, plantar fasciitis, trochanteric bursitis, De Quervain’s, etc.
• Ultrasound-guided injections for difficult-to-localize pain areas (improves precision and confidence)
All procedures are performed with strict sterile precautions, and guidance is used wherever it meaningfully improves safety and results. In short: less guesswork, more accuracy.
Biologics Therapy:
Biologic and targeted therapies can be genuinely life-changing in autoimmune and inflammatory arthritis, when matched correctly to the diagnosis and monitored properly. I guide patients through the entire process: who needs it, what to screen before starting, how to monitor, and how to use these safely long-term (including cost-effective options such as biosimilars where appropriate).
Common advanced therapies used in India
• Anti-TNF agents: Adalimumab, Etanercept, Infliximab, Golimumab
• IL-17 inhibitors: Secukinumab, Ixekizumab
• IL-12/23 and IL-23 inhibitors: Ustekinumab, Guselkumab
• B-cell therapy: Rituximab
• JAK inhibitors (JAKi): Tofacitinib, Baricitinib, Upadacitinib
Final choice always depends on diagnosis, severity, infection risk, comorbidities, and affordability.


Intra-articular Stem-Cell Therapy for Knee Osteoarthritis:
This is one of the newest and most “advanced” injection-based approaches being offered for knee OA. The goal is to reduce pain, improve function, and possibly delay surgery in selected patients.
That said, important honesty, stem-cell therapy is still an evolving field. Results vary because techniques and preparations differ across centres, and long-term evidence is still developing. So, I approach it in a patient-selection + transparent-expectations way. It is not suitable for everyone, especially in advanced/end-stage OA where mechanical damage dominates.
How I approach stem-cell therapy
• Discuss who is likely to benefit and who is not
• Explain realistic outcomes (pain/function improvement vs “cartilage regrowth claims”)
• Compare alternatives like physio, weight reduction, HA injections, PRP (if relevant), braces, and surgical options
• Discuss costs, safety, expected timeline, and follow-up plan
If it’s a good fit, it can be a valuable option, especially for people trying to avoid early knee replacement.
Synovial Fluid Replacement Therapy (Viscosupplementation):
Viscosupplementation is an injection of hyaluronic acid into the joint, most commonly the knee. Hyaluronic acid acts like a natural lubricant and shock absorber, which can help reduce pain and stiffness and improve day-to-day mobility in selected patients with osteoarthritis.
Why it can be important
• Helps patients who continue to have pain despite physiotherapy, strengthening, weight management, and routine medicines
• Can improve walking tolerance, stair climbing, and overall joint movement
• May help some patients delay knee replacement when surgery is not yet needed or not preferred
What results to expect
Relief varies from person to person. Many patients feel improvement for several months, and some longer, especially when combined with a structured plan of quadriceps strengthening and lifestyle measures.


Joint Injection / Aspiration:
This is one of the most useful tools in Rheumatology, because it can be both diagnostic and therapeutic.
Why aspiration/injection can be important (not “optional” in many cases)
• A swollen joint may represent infection, gout/pseudogout, inflammatory arthritis flare, or bleeding, and these need different treatments. In suspected infection, aspiration is critical, because injecting steroid without ruling out infection can be dangerous.
• Aspirating joint fluid can confirm the diagnosis quickly and prevent wrong treatment.
• Removing fluid can give immediate relief by reducing pressure inside the joint.
• Injections allow targeted treatment right where the inflammation is, often reducing the need for high-dose tablets.
Where it helps most
• Painful swollen knee/ankle/wrist/elbow/shoulder
• Sudden acute attacks (suspected gout / pseudogout)
• Persistent bursitis/tenosynovitis or frozen shoulder pain
• OA flare with significant joint inflammation
All procedures are done with strict sterile precautions, and ultrasound guidance is used where it improves accuracy and safety.
Osteoporosis & Bone Health Management:
Osteoporosis is one of the most underdiagnosed problems in adults, because it’s usually silent until a fracture happens. Many people first discover it after a wrist fracture, hip fracture, or spine (vertebral) compression fracture, which can permanently affect mobility and quality of life.
This service is focused on fracture prevention, early detection, and structured long-term treatment. Many people have osteoporosis for years without symptoms, so screening (DEXA scan) and risk assessment can prevent the first fracture.
How I help
• Risk assessment + fracture risk planning (not just a “calcium tablet” approach)
• Identifying secondary causes (many cases have reversible contributors)
• Planning exercise + nutrition + fall prevention
• Selecting the right medicine based on kidney function, fracture risk, and safety profile
• DEXA interpretation + fracture-risk planning
• Checking reversible causes (Vitamin D deficiency, thyroid/parathyroid issues, etc.)
Injectable osteoporosis therapies available (when indicated)
For moderate–high fracture risk patients, injectable therapies can be highly effective and practical:
• Zoledronic acid (ZA) (IV infusion, usually yearly)
• Denosumab (injection every 6 months)
• Teriparatide (bone-building injection; selected high-risk cases)
• Romosozumab (bone-building monthly injection for selected patients after cardiovascular risk assessment)
I also guide patients on the do’s and don’ts (timing, dental precautions, missed-dose handling, long-term planning), because these medicines work best when used correctly.


Chronic Pain Management:
Chronic pain is rarely “just pain.” It often involves a combination of factors, including joint degeneration, inflammation, nerve irritation, posture problems, muscle weakness, poor sleep, stress, vitamin deficiencies, or old injuries. If you only keep taking painkillers without finding the cause, pain tends to keep returning.
What chronic pain management actually does
• Identifies the root driver of pain (joint vs tendon vs nerve vs muscle vs inflammatory)
• Builds a plan to reduce pain and prevent recurrence, not just temporary relief
• Avoids long-term dependency on painkillers whenever possible
How I help
• Structured assessment to find the true source of pain
• Rational investigations only when needed (not “test-shopping”)
• Stepwise treatment plan: medicines (minimal necessary), targeted injections where appropriate, physio/strengthening, posture/ergonomics
• Guidance on activity modification so patients can return to function safely
• If a surgical opinion is needed, I’ll clearly tell you when and why, no dragging it out
Adult Vaccination:
Most adults assume vaccines are only for childhood. But as we grow older, and especially if we have diabetes, lung disease, heart disease, kidney disease, or autoimmune arthritis, vaccines become a simple, powerful way to prevent serious infections and hospitalisation.
This becomes even more important for patients who are (or may soon be) on steroids, biologics, or JAK inhibitors, because immunity can be lowered and infections can become more severe.
How I help
• Review your vaccine history and risk factors (age, comorbidities, travel, workplace exposure)
• Create a personalised adult vaccination plan
• Plan vaccine timing before starting immunosuppressive medicines whenever possible
• Guide which vaccines are safe during treatment, and which need special timing
Common adult vaccines we commonly discuss (based on your age & risk)
• Influenza (flu)
• Pneumococcal vaccine(s)
• COVID-19 boosters as per current recommendations
• Tdap/Td (tetanus–diphtheria ± pertussis boosters)
• Hepatitis B (and Hepatitis A in selected adults)
• Typhoid (TCV – Typhoid Conjugate Vaccine) in selected adults based on exposure risk/travel and local risk
• Hepatitis E vaccine in selected adults (especially when risk is high and vaccine availability is appropriate)
• Shingles (Herpes zoster) vaccine in older adults / higher-risk patients
• HPV (selected age groups / indications)
• MMR / Varicella only if non-immune and if timing is appropriate
• Travel vaccines (only when relevant)
Important safety note: some vaccines (live vaccines) may not be advisable while on strong immunosuppression, so timing matters. I’ll guide you through it properly so it’s safe and sensible.

