- For Appointment : +91-9330257079
- +91-9830636315
-
bodhi.doc@gmail.com
RHEUMATOLOGY
- Rheumatoid Arthritis
- Systemic Lupus Erythematosus
- Osteoarthritis
- Ankylosing Spondylitis
- Psoriatic Arthritis, Psoriasis
- Gout, Pseudogout
- Osteoporosis
- Spinal Stenosis
- Chronic back pain
- Reactive Arthritis
- Iritis/Uveitis
- Sjogren’s Syndrome
- Scleroderma/Systemic Sclerosis
- Mixed connective tissue disease
- Polymyositis/Dermatomyositis
- Fibromyalgia
- Juvenile Arthritis
- Tendinitis & Bursitis
- Plantar Fasciitis
- Tennis Elbow/Golfer’s Elbow
- Antiphospholipid Syndrome
- Carpal Tunnel Syndrome
- Polymyalgia rheumatica
- Paget’s Disease of Bone
- Raynaud’s Phenomenon
- Vasculitis
- Giant Cell Arteritis
- Wegener’s Granulomatosis
- HIV related Rheumatic Diseases
- HCV related Rheumatic Diseases
Rheumatoid Arthritis:
Fast Facts
Rheumatoid arthritis (RA) is the most common type of autoimmune arthritis. It is caused when the immune system (the body’s defense system) is not working properly. RA causes pain and swelling in the wrist and small joints of the hand and feet.
Treatments for RA can stop joint pain and swelling. Treatment also prevents joint damage. Early treatment will give better long term results.
Regular low-impact exercises, such as walking, and exercises can increase muscle strength. This will improve your overall health and lower pressure on your joints.
Studies show that people who receive early treatment for RA feel better sooner and more often, and are more likely to lead an active life. They also are less likely to have the type of joint damage that leads to joint replacement.
It is important to get the help of a rheumatologist. A rheumatologist is a doctor who treats arthritis and autoimmune disease. There are diseases that can be mistaken for RA. It is important to get the correct diagnosis without unnecessary testing. A rheumatologist will help find a treatment plan that is best for your disease.
People have long feared rheumatoid arthritis (commonly called RA) as one of the most disabling types of arthritis. The good news is that the outlook has greatly improved for many people with newly diagnosed (detected) RA. Of course, RA remains a serious disease, and one that can vary widely in symptoms (what you feel) and outcomes. Even so, treatment advances have made it possible to stop or at least slow the progression (worsening) of joint damage. Rheumatologists now have many new treatments that target the inflammation that RA causes. They also understand better when and how to use treatments to get the best effects.

What is rheumatoid arthritis?
RA is the most common form of autoimmune arthritis. About 75% of RA patients are women. In fact, 1 – 3% of women may get rheumatoid arthritis in their lifetime. The disease most often begins between the ages of 30
and 50. However, RA can start at any age.
RA is a chronic disease that causes joint pain, stiffness, swelling and decreased movement of the joints. Small joints in the hands and feet are most commonly affected. Sometimes RA can affect your organs, such
as eyes, skin or lungs.
The joint stiffness in active RA is often the worst in the morning. It may last one to two hours (or even the whole day). It generally improves with movement of the joints. Stiffness for a long time in the
morning is a clue that you may have RA, as this is not common in other conditions. For instance, osteoarthritis most often does not cause prolonged morning stiffness.
Other signs and symptoms that can occur in RA include:
• Loss of energy• Low fevers
• Loss of appetite
• Dry eyes and mouth from a related health problem,
• Firm lumps, called rheumatoid nodules, which grow beneath the skin in places such as the elbow and hands
What causes rheumatoid arthritis?
RA is an autoimmune disease. Your immune system is supposed to attack foreigners in your body, like bacteria and viruses, by creating inflammation. In an autoimmune disease, the immune system mistakenly sends inflammation to your own healthy tissue. The immune system creates a lot of inflammation that is sent to your joints causing joint pain and swelling. If the inflammation remains present for a long period of time, it can cause damage to the joint. This damage typically cannot be reversed once it occurs. The cause of RA is not known. There is evidence that autoimmune conditions run in families. For instance, certain genes that you are born with may make you more likely to get RA.
How is rheumatoid arthritis diagnosed?
RA is diagnosed by examining blood test results, examining the joints and organs, and reviewing x-ray or ultrasound images. There is no one test to diagnose RA. Blood tests are run to look for antibodies in the blood that can been seen in RA. Antibodies are small proteins in the bloodstream that help fight against foreign substances called antigens. Sometimes these antibodies are found in people without RA. This is called a false positive result. Blood tests are also run to look for high levels of inflammation. The symptoms of RA can be very mild making the diagnosis more difficult. Some viral infections can cause symptoms that can be mistaken for RA. A rheumatologist is a physician with the skill and knowledge to reach a correct diagnosis of RA and to recommend a treatment plan.
Abnormal blood tests commonly seen in RA include:
• Anemia (a low red blood cell count)
• Rheumatoid factor (an antibody, or blood protein, found in about 80% of patients with RA in time, but in as few as 30% at the start of arthritis)
• Antibodies to cyclic citrullinated peptides (pieces of proteins), or anti-CCP for short (found in 60 – 70% of patients with RA)
• Elevated erythrocyte sedimentation rate (a blood test that, in most patients with RA, confirms the amount of inflammation in the joints)
X-rays can help in detecting RA, but may be normal in early arthritis. Even if normal, initial X-rays may be useful later to show if the disease is progressing. MRI and ultrasound scanning can be done to help confirm or judge the severity of RA.
RA is a chronic arthritis. Generally, the symptoms will need to be present for more than three months to consider this diagnosis. However, there are patients who are diagnosed sooner.
How is rheumatoid arthritis treated?
Therapy for RA has improved greatly in the past 30 years. Current treatments give most patients good or excellent relief of symptoms and let them keep functioning at, or near, normal levels. With the right medications, many patients can have no signs of active disease. When the symptoms are completely controlled, the disease is in “remission”.
There is no cure for RA. The goal of treatment is to improve your joint pain and swelling and to improve your ability to perform day-to-day activities. Starting medication as soon as possible helps prevent your joints from having lasting or possibly permanent damage. No single treatment works for all patients. Many people with RA must change their treatment at least once during their lifetime.
RA patients should begin their treatment with disease-modifying antirheumatic drugs — referred to as DMARDs. These drugs not only relieve symptoms but also slow progression of the joint damage. Often, doctors prescribe DMARDs along with nonsteroidal anti-inflammatory drugs or NSAIDs and/or low-dose corticosteroids, to lower swelling and pain. DMARDs have greatly improved the pain, swelling, and quality of life for nearly all patients with RA. Ask your rheumatologist about the need for DMARD therapy and the risks and benefits of these drugs. Common DMARDs include – methotrexate, leflunomide, sulfasalazine & hydroxychloroquine.
Patients with more serious disease may need medications called biologic response modifiers or “biologic agents.” They can block immune system chemical signals that lead to inflammation and joint/tissue damage. Available drugs of this type include adalimumab, etanercept, infliximab &rituximab. Most often, patients take these drugs with methotrexate, as the mix of medicines is more helpful.
Janus kinase (JAK) inhibitors are another type of DMARD. People who cannot be treated with methotrexate alone may be prescribed a JAK inhibitor such as tofacitinib.
The best treatment of RA needs more than medicines alone. Patient education, such as how to cope with RA, also is important. Proper care often requires a team of providers, including rheumatologists, primary care physicians, and physical and occupational therapists. You will need frequent visits through the year with your rheumatologist. These checkups let your doctor track the course of your disease and check for any side effects of your medications. Also, you likely will need to repeat blood tests and X-rays or ultrasounds from time to time.
Living with rheumatoid arthritis
It is important to be physically active most of the time, but to sometimes scale back activities when the disease flares. In general, rest is helpful when a joint is inflamed, or when you feel tired. At these times, do gentle range-of-motion exercises, such as stretching. This will keep the joint flexible.
When you feel better, RA patients are encouraged to do low-impact aerobic exercises, such as walking, and exercises to boost muscle strength. This will improve your overall health and lower the pressure on your joints. A physical or occupational therapist can help you find which types of activities are best for you, and at what level or pace you should do them.
Finding that you have a chronic illness is a life-changing event. It can cause worry and sometimes feelings of isolation or depression. Thanks to greatly improved treatments, these feelings tend to decrease with time as energy improves, and pain and stiffness decrease. Discuss these normal feelings with your health care providers. They can provide helpful information and resources.
The rheumatologist’s role in the treatment of rheumatoid arthritis
RA is a complex disease, but many advances in treatment have occurred recently. Rheumatologists are doctors who are experts in diagnosing and treating arthritis and other diseases of the joints, muscles and bones. Thus, they are best qualified to make a proper diagnosis of RA. They can also advise patients about the best treatment options.
Systemic Lupus Erythematosus:

Fast Facts:
• Lupus occurs ten times more often in women than in men.
• Treatment depends on the organs involved.
• Involvement of the kidneys or/and the brain is the most serious manifestation of lupus.
• People can live well with lupus if they actively work toward good health.
• Sun exposure can lead to lupus flares.
• Carefully plan your pregnancies; lupus can flare during pregnancy and can affect its outcome.
Systemic lupus erythematosus, referred to as SLE or lupus, is a chronic (long-term) disease that causes systemic inflammation which affects multiple organs.
In addition to affecting the skin and joints, it can affect other organs in the body such as the kidneys, the tissue lining the lungs (pleura), heart (pericardium), and brain. Many patients experience fatigue, weight loss, and fever.
Lupus flares vary from mild to serious. Most patients have times when the disease is active, followed by times when the disease is mostly quiet – referred to as a remission. Yet, there is much reason for hope. Improvements in treatment have greatly improved these patients’ quality of life and increased their lifespan.
What causes lupus?
When healthy, our immune system protects the body from foreign germs and cancers. With lupus, the immune system misfires and attacks “self”, the patient’s own tissues, in a process called autoimmunity or “loss of self-tolerance”.
In lupus as the attack goes on, all the branches of the immune system join the fight. This leads to significant and intense inflammation. The cause of Lupus is unknown, as well as what drives its diverse presentation. We know that multiple factors are required, including: the “right” genetic makeup, environmental exposures, and organ specific characteristics. People with lupus may also have an impaired process for clearing old and damaged cells from the body, which in turn provides continuous stimuli to the immune system and leads to abnormal immune response.
Most often, lupus starts in young females in their fertility age.
How is lupus diagnosed?
Lupus can be hard to detect because it is a complex disease that has many symptoms, and they can come on slowly. As experts in diagnosing and treating autoimmune diseases such as lupus, rheumatologists can best
determine whether a patient has lupus and advise them about treatment options.
People with lupus often have symptoms that are not specific to lupus. These include fever, fatigue, weight loss, blood clots, and hair loss in spots or around the hairline. They may also have heartburn, stomach
pain, and poor circulation to the fingers and toes. Pregnant women can have miscarriages.
The American College of Rheumatology has a list of symptoms and other measures that doctors can use as a guide to decide if a patient with symptoms has lupus.
• Rashes:
∘ butterfly-shaped rash over the cheeks – referred to as malar rash
∘ red rash with raised round or oval patches – known as discoid rash
∘ rash on skin exposed to the sun
• Mouth sores: sores in the mouth or nose lasting from a few days to more than a month
• Arthritis: tenderness and swelling lasting for a few weeks in two or more joints
• Lung or heart inflammation: swelling of the tissue lining the lungs (referred to as pleurisy or pleuritis) or the heart (pericarditis), which can cause chest pain when breathing deeply
• Kidney problem: blood or protein in the urine, or tests that suggest poor kidney function
• Neurologic problem: seizures, strokes, or psychosis (a mental health problem)
• Abnormal blood tests such as:
∘ low blood cell counts: anemia, low white blood cells, or low platelets
∘
positive
antinuclear antibodies
(ANA) result:
antibodies that can cause the body to begin attacking itself that are present in nearly all lupus patients
∘ certain abnormal antibodies: anti-double-strand DNA (called anti-dsDNA), anti-Smith (referred to as anti-Sm), or antiphospholipid antibodies.
If your doctor suspects you have lupus based on your symptoms, a series of blood tests will be done in order to confirm the diagnosis. The most important blood screening test is ANA. If ANA is negative, you don’t have lupus. However, if ANA is positive, you might have lupus and will need more specific tests. These blood tests include antibodies to anti-dsDNA and anti-Sm, which are specific to the diagnosis of lupus.
The presence of antiphospholipid antibodies signals a raised risk for certain complications such as miscarriage or blood clots. Doctors also may measure levels of certain complement proteins (a part of the immune
system) in the blood, to help detect the disease and follow its progress
How is lupus treated?
Lupus is a chronic disease. The treatment objective is to induce remission. Treatment depends on the type of symptoms you have and how serious they are.
Common treatment options include:
• Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs decrease joint swelling, joint pain, fever, and inflammation of the heart and lung linings. These drugs include ibuprofen (brand names
Motrin, Advil) and naproxen (Naprosyn, Aleve). Some of these NSAIDs can cause serious side effects like stomach bleeding or kidney damage. Always check with your doctor before taking any medications that are over the
counter (without a prescription) for your lupus.
•
Antimalarial drugs:
Hydroxychloroquine recommended in every patient with lupus. Hydroxychloroquine was used in the past to prevent and treat malaria and found, during World War 2, to be effective for lupus related arthritis,
fatigue, rashes, and mouth sores.
•
Corticosteroids and immune suppressants:
Patients with serious or life-threatening problems such as kidney inflammation, lung or heart involvement, and central nervous system symptoms need more “aggressive” (stronger) treatment. This may include
high-dose corticosteroids such as prednisone and drugs that suppress the immune system. Immune suppressants include azathioprine, cyclophosphamide & cyclosporine. Recently mycophenolate mofetil has
been used to treat severe kidney disease in lupus – referred to as lupus nephritis.
•
Combination treatment:
Health care providers may combine a few medications to control lupus and prevent tissue damage. Each treatment has risks and benefits. Most immune-suppressing medications may cause side effects and require
close monitoring. Side effects of these drugs may include a raised risk of infections as well as nausea, vomiting, hair loss, diarrhea, high blood pressure, and osteoporosis (weak bones). Rheumatologists may
lower the dose of a drug or stop a medicine because of side effects or when the disease goes into remission. As a result, it is important to receive careful and frequent health exams and lab tests to track your
symptoms and change your treatment as needed
Broader health impact of lupus:
Lupus disease, especially when active, could lead to accelerated atherosclerosis (clogging of the arteries) which can develop in young women and could also lead to heart attacks, heart failure, and strokes. Thus, it is vital that patients with lupus, in addition to controlling their disease, exercise and lower other risk factors for heart disease, such as smoking, high blood pressure, and high cholesterol.
Renal inflammation is one of the common and most serious manifestations of lupus. It could go undetected and can lead to renal failure and dialysis. You can help prevent these serious outcomes by seeking treatment at the first signs of kidney disease.These signs include:
• High blood pressure
•Swollen feet and hands
• Puffiness around your eyes
•Changes in urination (blood or foam in the urine, going to the bathroom more often at night, or pain or trouble urinating)
Living with lupus:
Most people with lupus can live normal lives. Treatment of lupus has improved, and people with the disease are living longer.Here are a couple of tips that may help you when living with lupus:
•Form a support system: A good doctor-patient relationship and support from family and friends can help you cope with this chronic and often unpredictable illness.
•Get involved in your care: Learn as much as you can about lupus, your medications, and what kind of progress to expect. Take all your medications as your doctor prescribes, and visit your rheumatologist often to prevent serious problems. This lets your doctor keep track of your disease and change your treatment as needed. If you do not live near a rheumatologist, you may need to have your primary care doctor manage your lupus with the help of a rheumatologist.
•Stay active: Exercise helps keep joints flexible and may prevent heart disease and strokes. This does not mean overdoing it. Switch off doing light to moderate exercise with times of rest.
•Avoid excess sun exposure: Sunlight can cause a lupus rash to flare and may even trigger a serious flare of the disease itself. When outdoors on a sunny day, wear protective clothing (long sleeves, a big-brimmed hat) and use lots of sunscreen.
If you are a young woman with lupus and wish to have a baby, carefully plan your pregnancy. With your doctor’s guidance, time your pregnancy for when your lupus activity is low. While pregnant, avoid medications that can harm your baby. These include cyclophosphamide, cyclosporine, and mycophenolate mofetil. If you must take any of these medicines, or your disease is very active, use birth control. Rheumatologists have long been concerned that the female hormone estrogen or treatment with estrogen may cause or worsen lupus. Recent research showed that estrogen therapy can trigger some mild or moderate flares of lupus, but does not cause symptoms to get much worse. Yet, estrogen can raise the risk of blood clots. Thus, you should not take estrogen if your blood tests show antiphospholipid antibodies (meaning you already have a high risk of blood clots).
Osteoarthritis:
Fast Facts :
•Though some of the joint changes are irreversible, most patients will not need joint replacement surgery.
•OA symptoms (what you feel) can vary greatly among patients.
•A rheumatologist can detect arthritis and prescribe the proper treatment. The goal of treatment in OA is to reduce pain and improve function.
•Exercise is an important part of OA treatment, because it can decrease joint pain and improve function.
•At present, there is no treatment that can reverse the damage of OA in the joints. Researchers are trying to find ways to slow or reverse this joint damage.
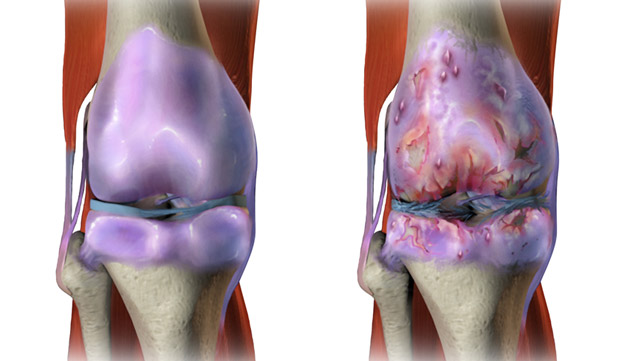
Osteoarthritis (also known as OA) is a common joint disease that most often affects middle-age to elderly people. It is commonly referred to as “wear and tear” of the joints, but we now know that OA is a disease
of the entire joint, involving the cartilage, joint lining, ligaments, and bone. Although it is more common in older people, it is not really accurate to say that the joints are just “wearing out.” It is
characterized by breakdown of the cartilage (the tissue that cushions the ends of the bones between joints), bony changes of the joints, deterioration of tendons and ligaments, and various degrees of inflammation
of the joint lining (called the synovium).
This arthritis tends to occur in the hand joints, spine, hips, knees, and great toes. The lifetime risk of developing OA of the knee is about 46%, and the lifetime risk of developing OA of the hip is 25%.
OA is a top cause of disability in older people. The goal of osteoarthritis treatment is to reduce pain and improve function. There is no cure for the disease, but some treatments attempt to slow disease
progression.
What is osteoarthritis?
OA is a frequently slowly progressive joint disease typically seen in middle-aged to elderly people. In osteoarthritis, the cartilage between the bones in the joint breaks down. This causes the affected bones to slowly get bigger. The joint cartilage often breaks down because of mechanical stress or biochemical changes within the body, causing the bone underneath to fail. OA can occur together with other types of arthritis, such as gout or rheumatoid arthritis.
OA tends to affect commonly used joints such as the hands and spine, and the weight-bearing joints such as the hips and knees.Symptoms include:
•Joint pain and stiffness
• Knobby swelling at the joint
• Cracking or grinding noise with joint movement
•Decreased function of the joint
Who gets osteoarthritis?
OA affects people of all races and both sexes. Most often, it occurs in patients age 40 and above. However, it can occur sooner if you have other risk factors (things that raise the risk of getting OA).Risk factors
include:
•Older age
•Having family members with OA
• Obesity
•Previous traumatic Joint injury or repetitive use (overuse) of joints
•Joint deformity such as unequal leg length, bowlegs or knocked knees
How is osteoarthritis diagnosed?
Rheumatologists are doctors who are experts in diagnosing and treating arthritis and other diseases of the joints, muscles and bones. You may also need to see other health care providers, for instance, physical or
occupational therapists and orthopedic doctors. Most often doctors detect OA based on the typical symptoms (described earlier) and on results of the physical exam. In some cases, X-rays or other imaging tests may be
useful to tell the extent of disease or to help rule out other joint problems.
How do you treat osteoarthritis?
There is no proven treatment yet that can reverse joint damage from OA. The goal of osteoarthritis treatment is to reduce pain and improve function of the affected joints. Most often, this is possible with a mixture
of physical measures and drug therapy and, sometimes, surgery.
•Physical measures: Weight loss and exercise are useful in OA. Excess weight puts stress on your knee joints and hips and low back. For every 10 pounds of weight you lose over 10 years, you can reduce the chance of developing knee OA by up to 50 percent. Exercise can improve your muscle strength, decrease joint pain and stiffness, and lower the chance of disability due to OA. Also helpful are support (“assistive”) devices, such as orthotics or a walking cane, that help you do daily activities. Heat or cold therapy can help relieve OA symptoms for a short time. Certain alternative treatments such as spa (hot tub), massage, and chiropractic manipulation can help relieve pain for a short time. They can be costly, though, and require repeated treatments. Also, the long-term benefits of these alternative (sometimes called complementary or integrative) medicine treatments are unproven but are under study.
•Drug therapy: Forms of drug therapy include topical, oral (by mouth) and injections (shots). You apply topical drugs directly on the skin over the affected joints. These medicines include capsaicin cream, lidocaine and diclofenac gel. Oral pain relievers such as acetaminophen are common first treatments. So are nonsteroidal anti-inflammatory drugs (often called NSAIDs), which decrease swelling and pain. Patients with more serious pain may need stronger medications, such as prescription narcotics. Joint injections with corticosteroids (sometimes called cortisone shots) or with a form of lubricant called hyaluronic acid can give months of pain relief from OA. This lubricant is given in the knee, and these shots may help delay the need for a knee replacement by a few years in some patients.
•Surgery: Surgical treatment becomes an option for severe cases. This includes when the joint has serious damage, or when medical treatment fails to relieve pain and you have major loss of
function. Surgery may involve arthroscopy, repair of the joint done through small incisions (cuts). If the joint damage cannot be repaired, you may need a joint replacement.
Supplements: Many over-the-counter nutrition supplements have been used for osteoarthritis treatment. Most lack good research data to support their effectiveness and safety. Among the most widely used are
calcium, vitamin D and omega-3 fatty acids. To ensure safety and avoid drug interactions, consult your doctor or pharmacist before using any of these supplements. This is especially true when you are combining these
supplements with prescribed drugs.
•Supplements : Many over-the-counter nutrition supplements have been used for osteoarthritis treatment. Most lack good research data to support their effectiveness and safety. Among the most widely used are calcium, vitamin D and omega-3 fatty acids. To ensure safety and avoid drug interactions, consult your doctor or pharmacist before using any of these supplements. This is especially true when you are combining these supplements with prescribed drugs.
Living with osteoarthritis:
There is no cure for OA, but you can manage how it affects your lifestyle.Some tips include:
•Properly position and support your neck and back while sitting or sleeping.
•Adjust furniture, such as raising a chair or toilet seat.
•Avoid repeated motions of the joint, especially frequent bending.
•Lose weight if you are overweight or obese, which can reduce pain and slow progression of OA.
•Exercise each day.
•Use adaptive devices that will help you do daily activities.
You might want to work with a physical therapist or occupational therapist to learn the best exercises and to choose arthritis assistive devices.
Ankylosing Spondylitis:
Fast Facts:
•Ankylosing spondylitis is a type of arthritis that attacks the spine and, in some people, the joints of the arms and legs. It can also involve the skin, intestines and eyes. The main symptom (what you feel) in most
patients is low back pain.
•In a minority of patients, the major symptom is pain and swelling in the arms and legs. This type is known as peripheral spondyloarthritis.
• People in their teens and 20s, particularly males, are affected most often. Family members of those with spondyloarthritis are at higher risk.
• Non-steroidal anti-inflammatory drugs (commonly called NSAIDs) offer symptom relief for most patients by reducing pain and swelling. Other medicines called anti-TNF drugs or TNF blockers are effective in patients who do not respond enough to NSAIDs.
• Newer treatments have helped a great deal in controlling symptoms, and frequent fitness activities and back exercises are helpful.
Spondyloarthritis (or spondyloarthropathy) is the name for a family of inflammatory rheumatic diseases that cause arthritis. It differs from other types of arthritis, because it involves the sites are where ligaments and tendons attach to bones called “entheses.” Symptoms present in two main ways. The first is inflammation causing pain and stiffness, most often of the spine. Some forms can affect the hands and feet or arms and legs. The second type is bone destruction causing deformities of the spine and poor function of the shoulders and hips. The most common is ankylosing spondylitis, which affects mainly the spine.
What causes ankylosing spondylitis?
Ankylosing spondylitis is hereditary. Many genes can cause it. Up to 30 of these genes have been found. The major gene that causes this disease is HLA-B27.
Who gets ankylosing spondylitis?
Ankylosing spondylitis tends to start in the teens and 20s and strikes males two to three times more often than females. Family members of affected people are at higher risk, depending partly on whether they inherited the HLA-B27 gene.
How is ankylosing spondylitis diagnosed?
Correct diagnosis requires a physician to assess the patient’s medical history and do a physical exam. The doctor also may order imaging tests or blood tests. You may need an X-ray of the sacroiliac joints, a pair of joints in the pelvis. X-ray changes of the sacroiliac joints, known as sacroiliitis, are a key sign of ankylosing spondylitis. If X-rays do not show enough changes, but the symptoms are highly suspicious, your doctor might order magnetic resonance imaging, or MRI, which shows these joints better and can pick up early involvement before an X-ray can.
Among the blood tests you may need is a test for the HLA-B27 gene. However, having this gene does not mean ankylosing spondylitis will always develop. Some people have the HLA-B27 gene but do not have arthritis and never develop arthritis. In the end, the diagnosis relies on the doctor’s judgment.
How is ankylosing spondylitis treated?
All patients should get physical therapy and do joint-directed exercises. Most recommended are exercises that promote spinal extension and mobility.
There are many drug treatment options. The first lines of treatment are the NSAIDs, such as naproxen, ibuprofen or indomethacin. No one NSAID is superior to another. Given in the correct dose and duration, these drugs give great relief for most patients.
For joint swelling that is localized (not widespread), injections, or shots, of corticosteroid medications into joints or tendon sheaths (the membrane around a tendon) can be effective quickly.
For patients who do not respond to the above lines of treatment, disease modifying antirheumatic drugs (commonly called DMARDs) such as sulfasalazine might be effective. These drugs relieve symptoms and may prevent damage to the joints. This class of drugs is helpful mainly in those with arthritis that also affects the joints of the arms and legs.
Although they may be effective, corticosteroids taken by mouth are not advised. This is because the high dose required will lead to many side effects.
Antibiotics are an option only for patients with reactive arthritis.
TNF alpha blockers (a newer class of drugs known as biologics) are very effective in treating both the spinal and peripheral joint symptoms of ankylosing spondylitis. TNF alpha blockers that has been approved for use in patients with ankylosing spondylitis are: adalimumab, infliximab & etanercept. However, anti-TNF treatment is expensive and not without side effects, including an increased risk for serious infections. Biologics can cause patients with latent tuberculosis (no symptoms) to develop an active infection.
Surgical treatment is very helpful in some patients. Total hip replacement is very useful for those with hip pain and disability due to joint destruction from cartilage loss. Spinal surgery is rarely necessary, except for those with traumatic fractures (broken bones due to injury) or to correct excess flexion deformities of the neck, where the patient cannot straighten the neck.
Broader health impacts:
Other problems can occur in patients with ankylosing spondylitis. You should discuss possible complications with your doctor.These can include:
• Osteoporosis , which occurs in up to half of patients with ankylosing spondylitis, especially in those whose spine is fused. Osteoporosis can raise the risk of spinal fracture.
•Inflammation of part of the eye, called uveitis, which occurs in about 40% of those with ankylosing spondylitis. Symptoms of uveitis include redness and pain of the eye. Steroid eye drops most often are effective, though severe cases may need other treatments from an ophthalmologist.
•Inflammation of the aortic valve in the heart, which can occur over time in patients with spondylitis. Your doctor should check your heart to make sure you do not have this problem.
•Psoriasis, a patchy skin disease, which if severe will need treatment by a dermatologist (skin doctor).
•Intestinal inflammation, which may be so severe that it requires treatment by a gastroenterologist (doctor who specializes in digestive diseases).
Living with ankylosing spondylitis:
Pain, fatigue and stiffness can be continuous or off and on. Despite these symptoms, most patients with ankylosing spondylitis lead productive lives and have a normal lifespan, especially with the newer treatments available. There are things you can do to improve your health. Frequent exercise is essential to maintain joint and heart health. If you smoke, try to quit. Smoking aggravates ankylosing spondylitis and can speed up the rate of spinal fusion. Patient support groups provide support and helpful information.
Psoriatic Arthritis:
Fast Facts:
•Psoriatic arthritis is a chronic arthritis. In some people, it is mild, with just occasional flare ups. In other people, it is continuous and can cause joint damage if it is not treated. Early diagnosis is important to avoid damage to joints.
•Psoriatic arthritis typically occurs in people with skin psoriasis, but it can occur in people without skin psoriasis, particularly in those who have relatives with psoriasis.
•Psoriatic arthritis typically affects the large joints, especially those of the lower extremities, distal joints of the fingers and toes, and also can affect the back and sacroiliac joints of the pelvis.
•For most people, appropriate treatments will relieve pain, protect the joints, and maintain mobility. Physical activity helps maintain joint movement.
Psoriatic arthritis is a type of inflammatory arthritis that occurs in some patients with psoriasis. This particular arthritis can affect any joint in the body, and symptoms vary from person to person. Research has shown that persistent inflammation from psoriatic arthritis can lead to joint damage. Fortunately, available treatments for are effective for most people.
Psoriatic arthritis usually appears in people between the ages of 30 to 50, but can begin as early as childhood. Men and women are equally at risk. Children with psoriatic arthritis are also at risk to develop uveitis (inflammation of the middle layer of the eye). Approximately 15% of people with psoriasis develop psoriatic arthritis. At times, the arthritis can appear before the skin disorder.
What is psoriatic arthritis?
Psoriasis is a disease in which scaly red and white patches develop on the skin. Psoriasis is caused by the body’s immune system going into overdrive to attack the skin. Some people with psoriasis can also develop psoriatic arthritis, manifested by painful, stiff and swollen joints. Like psoriasis, psoriatic arthritis symptoms flare and subside, vary from person to person, and even change locations in the same person over time.
Psoriatic arthritis can affect any joint in the body, and it may affect just one joint, several joints or multiple joints. For example, it may affect one or both knees. Affected fingers and toes can resemble swollen sausages, a condition often referred to as dactylitis. Finger and toe nails also may be affected.
Psoriatic arthritis in the spine, called spondylitis, causes stiffness in the back or neck, and difficulty bending. Psoriatic arthritis also can cause tender spots where tendons and ligaments join onto bones. This condition, called enthesitis, can result in pain at the back of the heel, the sole of the foot, around the elbows or in other areas. Enthesitis is one of the characteristic features of psoriatic arthritis.
Recent research suggests that persistent inflammation from psoriatic arthritis causes joint damage later, so early accurate diagnosis is essential. Fortunately, treatments are available and effective for most people
What causes psoriatic arthritis?
What causes psoriatic arthritis is not known exactly. Of those with psoriatic arthritis, 40% have a family member with psoriasis or arthritis, suggesting heredity may play a role. Psoriatic arthritis can also result from an infection that activates the immune system. While psoriasis itself is not infectious, it might be triggered by a streptococcal throat infection, commonly known as strep throat.
How is psoriatic arthritis diagnosed?
To diagnose psoriatic arthritis, rheumatologists look for swollen and painful joints, certain patterns of arthritis, and skin and nail changes typical of psoriasis. X-rays often are taken to look for joint damage. MRI, ultrasound or CT scans can be used to look at the joints in more detail.
Blood tests may be done to rule out other types of arthritis that have similar signs and symptoms, including gout, osteoarthritis, and rheumatoid arthritis. In patients with psoriatic arthritis, blood tests may reveal high levels of inflammation and mild anemia but labs may also be normal. Anemia is a condition that occurs when the body lacks red blood cells or has dysfunctional red blood cells. Occasionally skin biopsies (small samples of skin removed for analysis) are needed to confirm the psoriasis.
How is psoriatic arthritis treated?
Treating psoriatic arthritis varies depending on the level of pain, swelling and stiffness. Those with very mild arthritis may require treatment only when their joints are painful and may stop therapy when they feel better. Non-steroidal anti-inflammatory drugs are used as initial treatment.
If the arthritis does not respond, disease modifying anti-rheumatic drugs may be prescribed. These include sulfasalazine, methotrexate, cyclosporine and leflunomide. Sometimes combinations of these drugs may be used together. The anti-malarial drug hydroxychloroquine can help, but it usually is avoided as it can cause a flare of psoriasis. Azathioprine may help those with severe forms of psoriatic arthritis.
There are several biologic type medications available to treat psoriatic arthritis via infusion or injection.
The TNF Inhibitors such as adalimumab, etanercept and infliximab are also available and can help the arthritis as well as the skin psoriasis.
For swollen joints, corticosteroid injections can be useful. Surgery can be helpful to repair or replace badly damaged joints
Broader health impact of psoriatic arthritis:
The impact of psoriatic arthritis depends on the joints involved and the severity of symptoms. Fatigue and anemia are common. Some psoriatic arthritis patients also experience mood changes. Treating the arthritis and reducing the levels of inflammation helps with these problems. People with psoriasis are slightly more likely to develop high blood pressure, high cholesterol, obesity or diabetes. Maintaining a healthy weight and treating high blood pressure and cholesterol are also important aspects of treatment
Living with psoriatic arthritis:
Many people with arthritis develop stiff joints and muscle weakness due to lack of use. Proper exercise is very important to improve overall health and keep joints flexible. This can be quite simple. Walking is an excellent way to get exercise. A walking aid or shoe inserts will help to avoid undue stress on feet, ankles, or knees affected by arthritis. An exercise bike provides another good option, as well as yoga and stretching exercises to help with relaxation.
Some people with arthritis find it easier to move in water. If this is the case, swimming or walking laps in the pool offers activity without stressing joints. Many people with psoriatic arthritis also benefit from physical and occupational therapy to strengthen muscles, protect joints from further damage, and increase flexibility.
Gout:
Fast Facts:
•Intensely painful, swelling joints (most often in the big toe or other part of the foot) and/or bouts of arthritis that come and go may indicate gout.
•Finding the characteristic crystals in the fluid of joints allows health care providers to correctly diagnose gout.
• Gout treatments exist, but therapy should be tailored for each person. Treatment choices depend on kidney function, other health problems, personal preferences and other factors.
• Patients may need medications to lower their elevated blood uric acid levels that predispose to gout. The goal is a uric acid level less than 6 milligrams per deciliter (mg/dL).
•There are two types of medicine for gout. For control of acute attacks of joint pain, there are NSAIDs, colchicine and corticosteroids. After gout flares have resolved, there are medications that can lower the level of uric acid over time in order to prevent or lessen attacks.
•Lifestyle changes such as controlling weight, limiting alcohol intake and limiting meals with meats and fish rich in purines also can help control gout.
Gout is a painful and potentially disabling form of arthritis that has been around since ancient times. It is sometimes referred to as the “disease of kings,” because people long have incorrectly linked it to the kind of overindulgence in food and wine only the rich and powerful could afford. In fact, gout can affect anyone, and its risk factors vary.
The first symptoms usually are intense episodes of painful swelling in single joints, most often in the feet, especially the big toe. The swollen site may be red and warm. Fifty percent of first episodes occur in the big toe, but any joint can be involved. Fortunately, it is possible to treat gout and reduce its very painful attacks by avoiding food and medication triggers and by taking medicines that can help. However, diagnosing gout can be hard, and treatment plans often must be tailored for each person.
What causes gout?Gout occurs when excess uric acid (a normal waste product) collects in the body, and needle‐like urate crystals deposit in the joints. This may happen because either uric acid production increases or, more often, the kidneys cannot remove uric acid from the body well enough. Certain foods and drugs may raise uric acid levels and lead to gout attacks.These include:
•Shellfish and red meats
•Alcohol in excess
•Sugary drinks and foods that are high in fructose
•Some medications, such as:
∘low-dose aspirin (but because it can help protect against heart attacks and strokes, we do not recommend that people with gout stop taking low-dose aspirin)
∘certain diuretics (“water pills”) such as hydrochlorothiazide and furosemide
∘immunosuppressants used in organ transplants such as cyclosporine and tacrolimus
Over time, increased uric acid levels in the blood may lead to deposits of urate crystals in and around the joints. These crystals can attract white blood cells, leading to severe, painful gout attacks and chronic arthritis. Uric acid also can deposit in the urinary tract, causing kidney stones
Who gets gout?
Gout and its complications occur more often in men, women after menopause, and people with kidney disease. Gout is strongly linked to obesity, hypertension (high blood pressure), hyperlipidemia (high cholesterol and triglycerides) and diabetes. Because of genetic factors, gout tends to run in some families. Gout rarely affects children.
How is gout diagnosed?Some other kinds of arthritis can mimic gout, so proper diagnosis (detection) is key. Health care providers suspect gout when a patient has joint swelling and intense pain in one or two joints at first, followed by pain‐free times between attacks. Early gout attacks often start at night.
Diagnosis of gout can be made in several ways. Gout is often diagnosed upon the finding of uric acid based crystals. The physician may use a needle to extract fluid from an affected joint and will study that fluid under a microscope to find whether urate crystals are present. Crystals also can be found in deposits (called tophi) that can appear under the skin. These tophi occur in advanced gout.
Gout can also be diagnosed based on the pattern of joint involvement, characteristic symptoms, time course, blood tests for uric acid, and advanced imaging tests.
Uric acid levels in the blood are important to measure but can sometimes be misleading, especially if measured at the time of an acute attack. Levels may be normal for a short time or even low during attacks. Even people who do not have gout can have increased uric acid levels.
X-rays may show joint damage in gout of long duration. Ultrasound and dual energy computed tomography (commonly called dual energy CT) can show early features of gouty joint involvement. These imaging techniques also can help suggest the diagnosis
How is gout treated?Treatment of acute attacks:
One treatment for active gout flares is colchicine. This medicine can be effective if given early in the attack. However, colchicine can cause nausea, vomiting, diarrhea and other side effects. Side effects may be less frequent with low doses. Patients with kidney or liver disease, or who take drugs that interact (interfere) with colchicine, must take lower doses or use other medicines. Colchicine also has an important role in preventing gout attacks.
Nonsteroidal anti‐inflammatory drugs – commonly called NSAIDs – are aspirin‐like medications that can decrease inflammation and pain in joints and other tissues. High doses of short‐acting NSAIDs give the fastest relief of symptoms. These medicines may cause stomach upset, ulcers or diarrhea, but they are well tolerated by most people when used for the short term.
In patients with chronic undertreated gout crystals can be found in uric acid deposits (called tophi) that can damage joints & can appear under the skin. Corticosteroids, such as prednisone, methylprednisolone, and triamcinolone,
are useful options for patients who cannot take NSAIDs. Given orally (by mouth) or by injection (shot) into the muscle, these medicines can be very effective in treating gout attacks. If only one or two joints are involved, your doctor
can inject a corticosteroid directly into your joint.
Some home remedies may help ease gout pain and reduce flares. Cherry products such as whole cherries or unsweetened cherry juice may reduce gout flares. A glass of skim milk daily may also help to lower uric acid over time. During an
attack, rest the affected joint and apply ice packs or cold compresses (cloths soaked in ice water and wrung out) to that spot.
Treatment to remove excess uric acid:
Patients who have repeated gout flares, abnormally high levels of blood uric acid, or tophi or kidney stones should strongly consider medicines to lower blood uric acid levels. These medications do not help the painful flares of acute gout, so most patients should start taking them after acute attacks subside. The drugs most often used to return blood levels of uric acid to normal is allopurinol & febuxostat. They block production of uric acid.
Probenecid help the kidneys remove uric acid. Only patients with good kidney function who do not overproduce uric acid should take these therapies.
Gout flares often can occur when you first start to use medications that lower blood uric acid levels. Patients can help prevent flares when starting these medications by also using low‐dose colchicine or NSAIDs. Often, doctors advise patients to keep taking colchicine in a low, preventive dose together with the uric acid-lowering medicine for at least six months.
If you are taking a uric acid-lowering drug, your doctor should slowly raise the dose and keep checking your blood uric acid levels. Once your uric acid levels drop below 6 mg/dL (normal), crystals tend to dissolve and new deposits of crystals can be prevented. You probably will have to stay on this medicine long term to prevent gout attacks.
What works well for one person may not work as well for another. Therefore, decisions about when to start treatment and what drugs to use should be tailored for each patient. Treatment choices depend on kidney function, other health problems, personal preferences and other factors.
What you eat can increase uric acid levels. Limit the amount of high-fructose drinks, such as non-diet soda. Also, do not drink alcohol, especially beer. Restrict eating foods that are rich in purines, compounds that break down into uric acid. These compounds are high in meat and certain types of seafood. New research has found purines in vegetables appear to be safe. Low‐fat dairy products may help lower uric acid levels.
In almost all cases, it is possible to successfully treat gout and bring a gradual end to attacks. Treatment also can decrease the number and size of tophi (deposits of uric acid crystals).
Broader health impacts of gout:Gout often is associated with high blood pressure, heart and kidney disease, or the use of medications that increase uric acid levels. Therefore, health care providers should test for these related health problems. Researchers are studying whether lowering blood uric acid levels can help heart disease and kidney disease.
Living with gout:Gout affects quality of life by both the intermittent attacks and the potential for chronic (lasting) arthritis. Compliance with your treatment plan is critical. Lifestyle changes may make it easier to manage this lifelong disease. Suggestions include gradual weight loss, avoidance of alcohol and reduced consumption of fructose‐containing drinks and foods high in purines.
