- For Appointment : +91-9330257079
- +91-9830636315
-
bodhi.doc@gmail.com
Fast Facts :
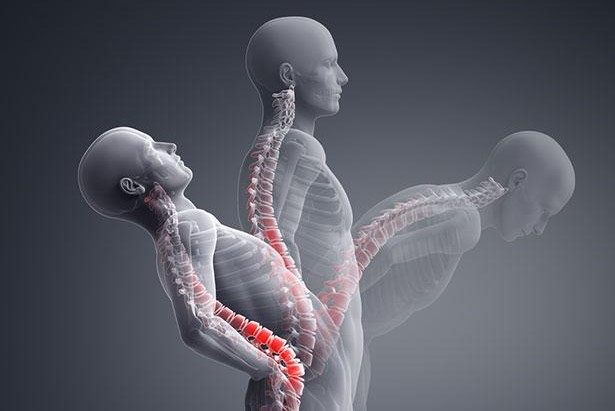
>>Ankylosing spondylitis is a type of arthritis that attacks the spine and, in some people, the joints of the arms and legs. It can also involve the skin, intestines and eyes. The main symptom (what you feel) in most patients is low back pain.
>>In a minority of patients, the major symptom is pain and swelling in the arms and legs. This type is known as peripheral spondyloarthritis.
>>People in their teens and 20s, particularly males, are affected most often. Family members of those with spondyloarthritis are at higher risk.
>>Non-steroidal anti-inflammatory drugs (commonly called NSAIDs) offer symptom relief for most patients by reducing pain and swelling. Other medicines called anti-TNF drugs or TNF blockers are effective in patients who do not respond enough to NSAIDs.
>>Newer treatments have helped a great deal in controlling symptoms, and frequent fitness activities and back exercises are helpful.
Spondyloarthritis (or spondyloarthropathy) is the name for a family of inflammatory rheumatic diseases that cause arthritis. It differs from other types of arthritis, because it involves the sites are where ligaments and tendons attach to bones called "entheses." Symptoms present in two main ways. The first is inflammation causing pain and stiffness, most often of the spine. Some forms can affect the hands and feet or arms and legs. The second type is bone destruction causing deformities of the spine and poor function of the shoulders and hips. The most common is ankylosing spondylitis, which affects mainly the spine.
What causes ankylosing spondylitis?
Ankylosing spondylitis is hereditary. Many genes can cause it. Up to 30 of these genes have been found. The major gene that causes this disease is HLA-B27.
Who gets ankylosing spondylitis?
Ankylosing spondylitis tends to start in the teens and 20s and strikes males two to three times more often than females. Family members of affected people are at higher risk, depending partly on whether they inherited the HLA-B27 gene.
How is ankylosing spondylitis diagnosed?
Correct diagnosis requires a physician to assess the patient's medical history and do a physical exam. The doctor also may order imaging tests or blood tests. You may need an X-ray of the sacroiliac joints, a pair of joints in the pelvis. X-ray changes of the sacroiliac joints, known as sacroiliitis, are a key sign of ankylosing spondylitis. If X-rays do not show enough changes, but the symptoms are highly suspicious, your doctor might order magnetic resonance imaging, or MRI, which shows these joints better and can pick up early involvement before an X-ray can.
Among the blood tests you may need is a test for the HLA-B27 gene. However, having this gene does not mean ankylosing spondylitis will always develop. Some people have the HLA-B27 gene but do not have arthritis and never develop arthritis. In the end, the diagnosis relies on the doctor's judgment.
How is ankylosing spondylitis treated?
All patients should get physical therapy and do joint-directed exercises. Most recommended are exercises that promote spinal extension and mobility.
There are many drug treatment options. The first lines of treatment are the NSAIDs, such as naproxen, ibuprofen or indomethacin. No one NSAID is superior to another. Given in the correct dose and duration, these drugs give great relief for most patients.
For joint swelling that is localized (not widespread), injections, or shots, of corticosteroid medications into joints or tendon sheaths (the membrane around a tendon) can be effective quickly.
For patients who do not respond to the above lines of treatment, disease modifying antirheumatic drugs (commonly called DMARDs) such as sulfasalazine might be effective. These drugs relieve symptoms and may prevent damage to the joints. This class of drugs is helpful mainly in those with arthritis that also affects the joints of the arms and legs.
Although they may be effective, corticosteroids taken by mouth are not advised. This is because the high dose required will lead to many side effects.
Antibiotics are an option only for patients with reactive arthritis.
TNF alpha blockers (a newer class of drugs known as biologics) are very effective in treating both the spinal and peripheral joint symptoms of ankylosing spondylitis. TNF alpha blockers that has been approved for use in patients with ankylosing spondylitis are: adalimumab, infliximab & etanercept. However, anti-TNF treatment is expensive and not without side effects, including an increased risk for serious infections. Biologics can cause patients with latent tuberculosis (no symptoms) to develop an active infection.
Surgical treatment is very helpful in some patients. Total hip replacement is very useful for those with hip pain and disability due to joint destruction from cartilage loss. Spinal surgery is rarely necessary, except for those with traumatic fractures (broken bones due to injury) or to correct excess flexion deformities of the neck, where the patient cannot straighten the neck.
Broader health impacts:
Other problems can occur in patients with ankylosing spondylitis. You should discuss possible complications with your doctor.These can include:
>>Osteoporosis, which occurs in up to half of patients with ankylosing spondylitis, especially in those whose spine is fused. Osteoporosis can raise the risk of spinal fracture.
>>Inflammation of part of the eye, called uveitis, which occurs in about 40% of those with ankylosing spondylitis. Symptoms of uveitis include redness and pain of the eye. Steroid eye drops most often are effective, though severe cases may need other treatments from an ophthalmologist.
>>Inflammation of the aortic valve in the heart, which can occur over time in patients with spondylitis. Your doctor should check your heart to make sure you do not have this problem.
>>Psoriasis, a patchy skin disease, which if severe will need treatment by a dermatologist (skin doctor).
>>Intestinal inflammation, which may be so severe that it requires treatment by a gastroenterologist (doctor who specializes in digestive diseases).
Living with ankylosing spondylitis:
Pain, fatigue and stiffness can be continuous or off and on. Despite these symptoms, most patients with ankylosing spondylitis lead productive lives and have a normal lifespan, especially with the newer treatments available. There are things you can do to improve your health. Frequent exercise is essential to maintain joint and heart health. If you smoke, try to quit. Smoking aggravates ankylosing spondylitis and can speed up the rate of spinal fusion. Patient support groups provide support and helpful information.
